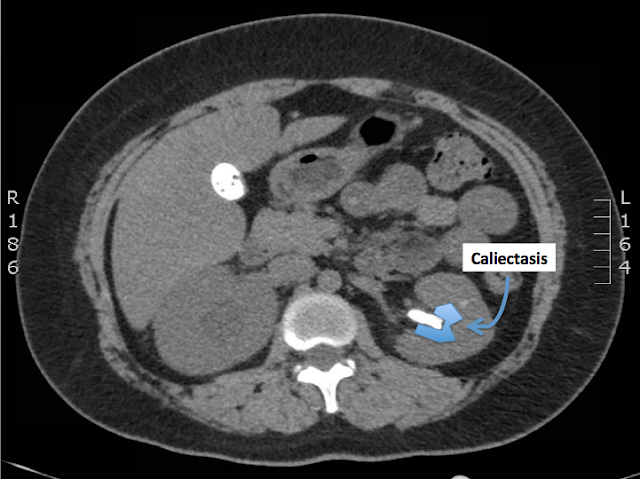
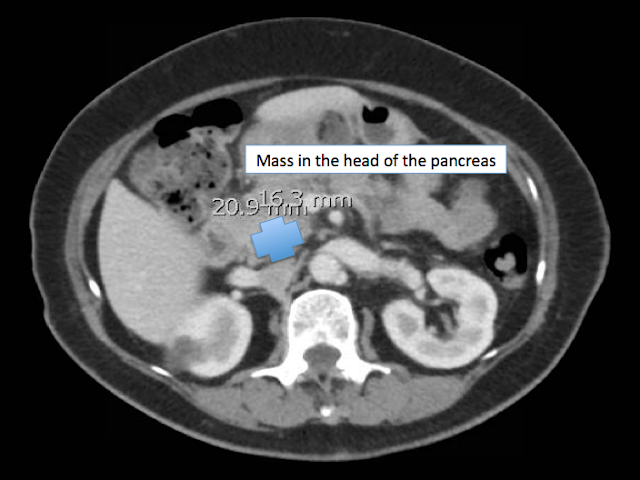
The patient's CT urogram showed bilateral nephrolithiasis with a large obstructing calculus in the right ureteropelvic junction with associated moderate hydronephrosis.
There is also a large staghorn calculus in the mid-to-upper pole of the left kidney, associated with severe left upper pole caliectasis.
The patient underwent interventional radiology-guided right nephrostomy tube placement without complication. Following the procedure the patient's pain improved, was able to tolerate po and ambulate. She was discharged 2 days later.
Nephrolithiasis
Epidemiology
- typically adults ages 20-50 years old
- 3:1 male:female ratio
- most stones are calcium oxalate or mixed calcium oxalate and phosphate
- less common: struvite (magnesium-ammonium phosphate --> urea-splitting bacteria)
- Proteus, Klebsiella, Pseudomonas
- less common: uric acid (i.e. gout)
- 90% of stones < 5mm will pass spontaneously (> 5mm unlikely to pass)
- 40% of symptomatic patients will have a recurrence
Pathogenesis
- urine becomes supersaturated with a particular mineral
- poor oral intake or excessive urinary losses
- excess secretion of a mineral (i.e. hypercalciuria, hyperoxaluria)
- stones form in renal collecting system and pass into ureter
Clinical Features
- abrupt onset of flank pain, radiates to abdomen and groin
- nausea and vomiting are common
- patient often unable to find a comfortable position
- fever is atypical --> consider alternative diagnoses if present
- abdomen usually nontender; consider abdominal aortic aneurysm if pulsatile mass palpated or bruit auscultated
- costovertebral angle tenderness is inconsistent
Urinanalysis
- hematuria usually present, about 15% however will not have hematuria
- WBCs and bacteria should raise concern for infection
- pH >7.6 = concern for struvite and urea-splitting bacteria
Blood work
- CBC and electrolytes typically are normal
- BUN and Creatinine are usually normal even in context of obstructive uropathy if other kidney is functioning
- Check calcium
**Rule out vascular catastrophe! (i.e. AAA, iliac aneurysm, etc)**
Imaging
- CT urogram = gold standard
- sensitive and specific, can measure degree of obstruction if present, may detect alternative diagnoses, no IV contrast needed
- US
- great for detecting and measuring renal obstruction, can detect stones in the kidneys, often misses stones in the ureters
Management
- analgesia with NSAIDs (first-line), opioids, or both
- antiemetics
- IV hydration
- alpha-blocking agents such as Tamulosin to aid stone passage is controversial (currently recommended by the American Urological Association)
- absolute indications for admission:
- intractable nausea and vomiting, or intractable pain
- obstruction with infection
- relative indications for admission:
- stone >5 mm
- high-grade obstruction
- solitary kidney
- deteriorating renal function
References:
Lopez BL, Brooks M, Emergency Medicine: A Focused Review of the Core Curriculum, 1st Ed, 2008, Chapter 17: Renal and Urological Disorders, pages 989-994
Discite Exerceo Adservio